Los Altos Optometric Group
Your Eye Clinic in Los Altos, California
The eye care services at Los Altos Optometric Group in Los Altos, California go above and beyond routine check-ups and updated vision prescriptions. Whether you visit our Los Altos optometrists for a visual acuity test, comprehensive eye exam, contact lens fitting, designer eyeglasses or treatment for an eye disease or condition, you’ll benefit from our expert skill and excellent patient service.

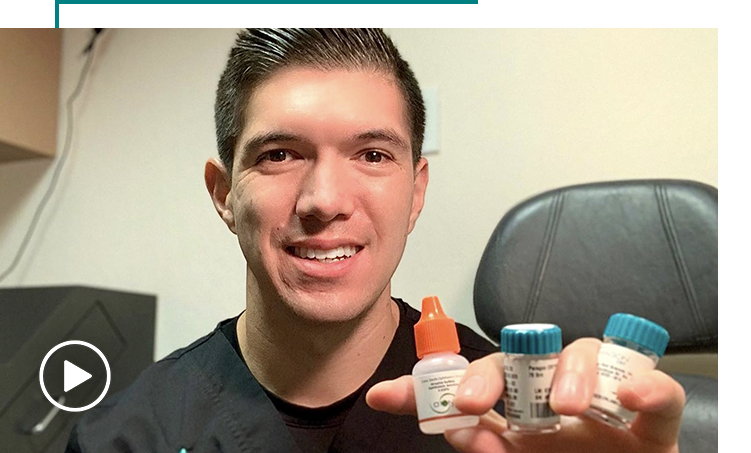
Dr. Aaron Neufeld
Born and raised in the Bay Area, Dr. Neufeld obtained his B.S. in Biology from UCLA and his O.D. degree from Southern College of Optometry, where he graduated with honors.

Dr. Matthew Tran
Dr. Tran was born and raised in San Jose, CA. He attended the University of San Francisco with a B.S. in Biology and minor in Chemistry. He received his Doctor of Optometry degree from the Southern California College of Optometry at Marshall B. Ketchum University.
Patient Reviews